Transdermal Patch Testing Equipment is the quiet engine behind trustworthy in-vitro data for patches, creams, ointments, and gels. As a manufacturer, Raytor designs and builds systems that reduce variability, shorten test cycles, and deliver data you can defend. Our perspective is simple: instruments should remove manual error, enforce pharmacopoeial compliance, and make your team faster without sacrificing rigor.

Why Transdermal Patch Testing Equipment Matters for R&D
Regulatory expectations have risen. Reviewers want proof of method robustness, complete traceability, and tight environmental control. Many labs still rely on manual sampling, mixed hardware, and makeshift thermostats. The result is variable diffusion profiles, bubble formation, and temperature drift that inflate repeat work and delay submissions.
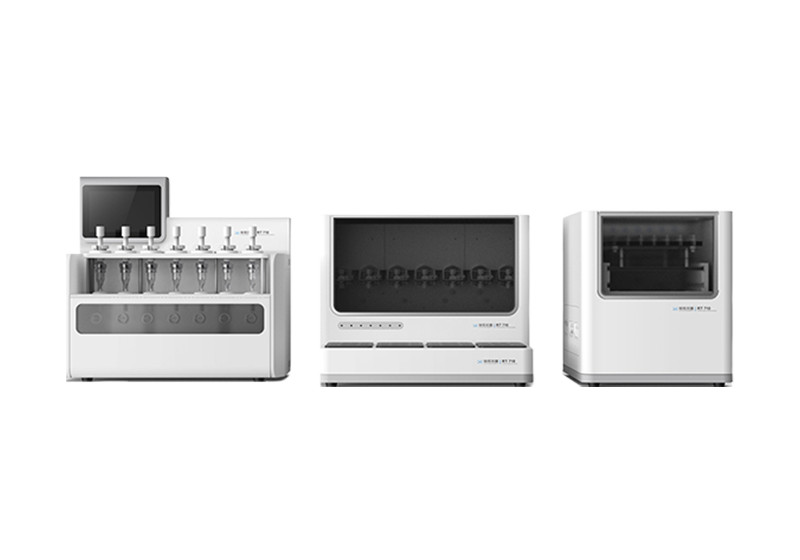
Raytor addresses these pain points with an automated Franz diffusion cell system built around modular design. The integrated diffusion cell device, automatic sampling module, and a medium thermostat work as one. Independent temperature control for every cell keeps tests on spec, while real-time monitoring and recording secure your audit trail. The system's mechanical tilt and automatic bubble removal cut operator influence and stabilize early-time points - often the noisiest region of a release curve. In short, Transdermal Patch Testing Equipment should standardize your day, not complicate it.
✅ What Sets Raytor's Approach Apart
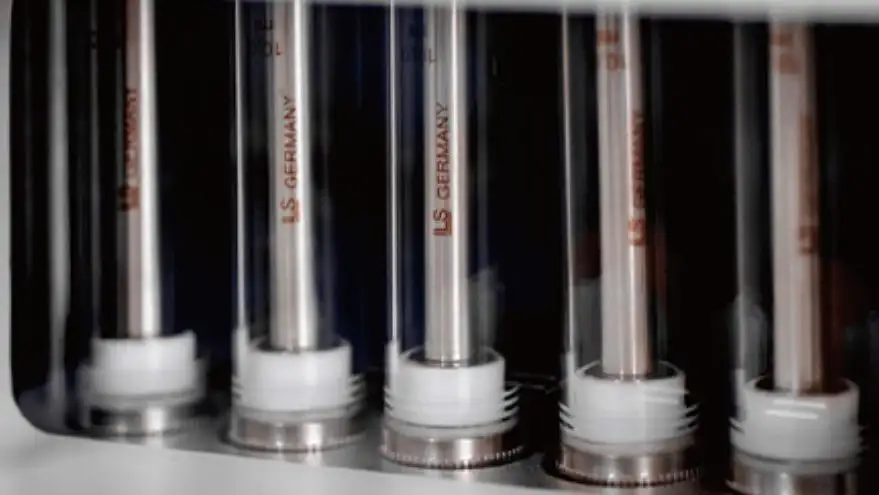
Our integrated glass diffusion cells reduce leakage risk during long runs. Separate pipelines and dedicated pumps for each cell prevent cross-contamination. Two independent groups of cells allow parallel studies without interference. Flexible sampling - partial or full - matches your protocol, whether you run quick screening or extended release.
Inside Raytor's Transdermal Patch Testing Equipment
At the core is a fully automatic 14-position transdermal diffusion cell (Franz cell) system. Automation controls stirring, temperature, and sampling schedules. The mechanical structure can tilt cells to purge residual bubbles in real time, minimizing human variability and protecting your early data points. Independent control per position makes method transfer smoother across sites and batches. Real-time monitoring and continuous recording support data integrity from start to finish.

1) Key Capabilities at a Glance
•14 diffusion cell positions arranged as 7x2 for parallel studies
•Independent temperature control per cell; room temperature to 50 °C (dry heating)
•Temperature error < ±0.5 °C for tight thermal control
•Stirring speed range 200–900 rpm; speed error < ±10%
•Automatic sampling with up to 24 time points per run
•Sampling range 1–10 mL, supporting full or partial sampling methods
•Maximum sampling time up to 9,999 minutes for extended profiles
•Integrated glass diffusion cells to reduce leakage risk
•Automatic bubble removal via real-time tilt and exhaust
•Separate pipelines and dedicated pumps to avoid cross-contamination
2) Applications Aligned with USP <1724>
The system meets the test requirements of the European Pharmacopoeia (EP 9.0) General Chapter <2.9.4> Dissolution test for transdermal patches and the United States Pharmacopeia General Chapter <1724> Semisolid Drug Products - Performance Tests. It supports in vitro release and permeation testing for creams, ointments, patches, and gels. For teams standardizing on in vitro permeation testing equipment, this compliance reduces method rework and speeds QA sign-off.
Practical Workflow and Data Quality Tips
Successful diffusion testing begins before you press “start.” Define the sampling plan around your formulation's expected release kinetics - dense ointments often need more early time points, while thin gels may benefit from steadier mid-phase intervals. Use partial sampling to preserve sink conditions when your analyte is highly soluble; use full sampling when mass balance and simple analysis pipelines are priorities.
When loading membranes, keep handling consistent across positions. The integrated structure helps here by minimizing assembly variation and leakage. Match stirring speeds to viscosity to prevent vortexing and micro-eddies that affect boundary layers. With independent temperature control, align each position to your target and verify equilibration before the first draw.
✅ Best Practices for Reliable Results with Transdermal Patch Testing Equipment
•Lock protocols to pharmacopoeial chapters (EP 9.0 <2.9.4>, USP <1724>) to streamline review
•Use the automated Franz diffusion cell system to remove operator-to-operator variation
•Select partial or full sampling per method goals; document rationale in your SOP
•Exploit real-time monitoring to flag drift early; pause and correct instead of repeating runs
•Keep separate pipelines pristine to prevent carryover, especially with potent actives
From an operational view, the ability to run two independent groups supports A/B method comparisons or parallel stability pulls. This is valuable when you must compare adhesives, backings, or drug load variations under identical conditions. Choosing cell volumes (9, 10, or 12 mL) to fit solubility and assay sensitivity further strengthens data quality. When your team can configure once and execute many, cycle times drop and analyst attention shifts to science over setup.
CTA - Ready to accelerate your topical and patch studies?
Talk to a Raytor specialist about configuring Transdermal Patch Testing Equipment for your current SOPs and upcoming submissions. We'll review your matrices, propose sampling schedules, and help you validate under EP and USP guidance - so you can move from draft method to defendable report with fewer repeats.